In Malta, around 10% of the local population is affected by diabetes. This is especially alarming considering that diabetes can affect the blood and nervous system and eventually even lead to foot amputations. Researchers from the University of Malta (UM) and Mater Dei Hospital are trying to address this problem in their project Sit_Diab: Smart Insole Technology for the Diabetic Foot. They developed a novel method of detecting foot complications early enough to take action in time to help save limbs.
Continue readingCaring for Carers
Parkinson’s disease (PD) is a complex, progressive, neurodegenerative condition affecting around 10 million people worldwide. But for every person directly struggling with PD, there is at least one carer, if not an entire family, dedicated to managing the disease. Are we doing enough to support these silent heroes? Cassi Camilleri asks.
‘I’m extremely anxious about her balance. Since the diagnosis, it’s been a constant nightmare because of the risk of falling and getting hurt. In reality, it’s only now that it’s started to become slightly affected,’ says Mildred Atanasio.
Mildred’s mother Rita was diagnosed with PD some years back after her husband passed away. One evening, Rita picked up one of her favourite novels for an evening read and noticed a tremor in her hand.
‘The worst part is when she tells me that all is ok and lovingly attempts to disguise a PD-caused stumble as something less worrying,’ Mildred continues.
‘She does this out of love, we know. She is worried about being a burden on me or my siblings, an idea which cannot be further from the truth. We all love her just the way she is. But this, coupled with my own fear and worry is rather draining… though I think sometimes my mind is worse than the actual symptoms.’
Though her experience is unique in many ways, the feeling of anxiety Mildred goes through is one she shares with many others.
The task of caring for another human being requires time and energy. According to the European Parliament Interest Group on Carers (EPIGC), carers spend an average of 22 hours per week providing for their loved ones. Even when this is done willingly and with love, without the right support network, it can leave carers susceptible to significant strains on their own physical, mental, and emotional health.
The same research by the EPIGC reveals that a third of carers lack sleep and feel depressed. Another third say that they are at a ‘breaking point’; one in five is unable to see anything positive in their life.
Close relatives often take on this important role; however, they often reject the term ‘carer’, seeing their work as a natural extension of the relationship with their affected loved one. ‘I am a daughter first. And the word ‘carer’ does not quite fit in my mental image of things,’ Mildred explains.
However, this has seen many go unrecognised for the service they provide for our community. Often, those who do not register themselves as carers are less likely and less able to access the services available to them.
You are not alone
Working hard to reverse this trend is the Malta Parkinson’s Disease Association (MPDA), with Veronica Clark at the helm as president.
MPDA informs citizens about PD and offers practical help on how to manage symptoms in the home. This includes talks by healthcare professionals so that people with PD and their carers are empowered to better manage their condition.
Peer support meetings foster a discussion about emotional and psychological needs and allow carers to cope with mental health issues they might be facing. Healthcare professionals are employed to further achieve this.
Mildred and her family make use and speak highly of these services. ‘Thanks to the MPDA, we have discovered and happily become part of a strong network of friends,’ Mildred says, a network she describes as very comforting. ‘We also share useful tips among us for day-to-day life which is nice.’
Giving a snapshot of the situation in Malta, Clark is quick to point out the benefits of our national healthcare system, which provides free treatment, accessible to people with Parkinsons in a whole range of disciplines, from neurologists and GPs to physiotherapists, speech therapists, occupational therapists. All this eases pressure on families and carers like Mildred and many others.
Malta also gives access to most PD medications through the government free at the point of use. The same can be said when it comes to any required surgery. This is available ‘without the need to travel,’ Clark specifies, ‘and this is also free, which I will point out is not the case for all European countries.’
An important role the MPDA has is its dissemination of information on how to access support services which may be required outside the family network. The Active Ageing community, Clark tells us, provides services like a carer at home, meals on wheels, home help, and many more. ‘Some aids are free and some are subsidised,’ Clark explains. ‘It is so important that people know they are not alone.’
Dancing to better health
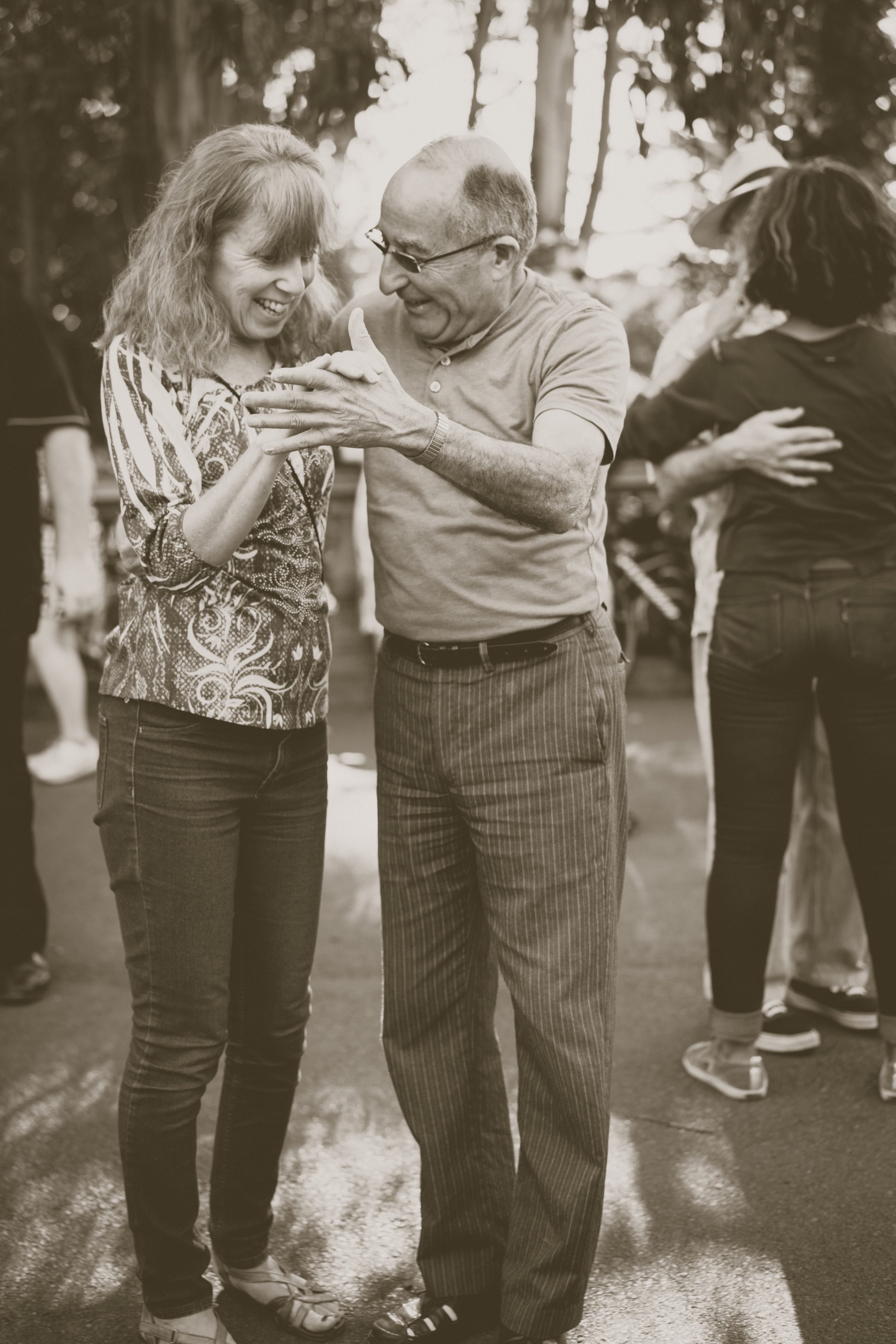
Mildred has nothing but wonderful things to say about a special group the MPDA introduced her to — Step Up for Parkinson’s (SUFP).
SUFP are not only dance classes for people with PD and their carers, but a community of people dedicated to uplifting one another.
Dancer Natalie Muschamp founded the organisation around 2016 and hasn’t looked back since.The binding philosophy is to help maintain physical activity of motor movement through dance, all while allowing the person with PD and their carer to bond and enjoy doing something together that isn’t about service.
‘When you have a disease or become a carer, you can lose your identity,’ Muschamp explains. ‘When [our participants] come to the class, they’re just two people and not a sick person and someone taking care of them. We sometimes even separate the couples. We put a lot of emphasis on this. And we encourage them to live their own lives. Some people, even after losing their partners, they continue to come. They regain some of their agency here.’
Of course, there is always room for improvement.
A concern Clark, Mildred, and Muschamp all have is that there are no specialised services tailored specifically for PD — neurologists, PD nurses, therapists, etc.
‘The lack of PD awareness people have at first hand’ is another point Mildred brings up. ‘There are so many misconceptions surrounding the condition,’ she said, ‘which often lead to added difficulties for people with Parkinson’s. To give a few examples, non-motor symptoms, such as hallucinations and impulsivity may easily lead to conflicts within the family unless they are recognised and understood. Slowness and rigidity may force people with Parkinson’s to take longer to cross the road or pay at the counter, leading to undeserved frowns or the tendency of rushing them, often quite unkindly.’
The fact that so many people don’t know what it is like to live with PD creates isolation and damaged relationships across the board. ‘The system needs to address not only the physical part of PD but also the mental, emotional, and social burdens it carries,’ Mildred encourages.
And while both MPDA and SUFP are doing their best to keep making positive changes, there is no escaping the biggest hurdle of all.
‘Co-ordinating regular and timely sessions between health professionals (from both the private and public sector) for people with PD is quite a challenge, due to reduced resources,’ explains Clark. ‘This means leaving people waiting longer or not receiving the regularity of sessions they need to manage their condition.’
The COVID effect
SUFP are also struggling with funding, especially as classes cannot happen in the real world anymore. ‘A lot of our participants struggle with the online thing,’ she explains, ‘and it’s worrying.’
‘For us not going to the gym, it will have an effect on our jean size. But for people suffering with Parkinson’s, it’s much more than that. Some of our participants started declining,’ she reveals sadly.
Ever adapting and creative, Muschamp tried to go around this by repurposing the footage from a cancelled tour with SUFP participants performing in shows all around Malta into a feature length documentary called One Day We Will Dance Again and a TV show called Step Up.
The show will air on ONE TV from January through to June of 2021, providing 15 minutes of daily exercises for the elderly and people with disabilities. ‘Amy, Mildred, Michelle, Roberta, Rowanne, myself, and everyone else — we’re currently in the middle of filming at the moment. Now we just need a good handful of sponsors to come forward — we have adverts to sell!’ she laughs, slapping the table, determined as always.
Knowing full well how infectious her energy is, Muschamp explains where it stems from — community. ‘These people are my people. My family,’ she says. ‘I can’t stop.’
The same goes for Clark. ‘When we see a smile on everyone’s face every month during our [MPDA] meetings, we know that the work we do is meaningful, and this really pushes us to continue to do what we do well,’ she says.
‘It is crucial not to live with PD alone,’ Mildred says, ‘be it the diagnosed person or the one accompanying them, whatever the stage of PD. Get in touch with the MPDA. The committee will be happy to assist them and direct them to any professional healthcare that they may require. And go to the dance classes when they start again. It makes a difference.’
‘We have to remember the bigger picture,’ Muschamp asserts. ‘What if the carer disappears? What if something bad happens to them? What then? The person with PD would need to be institutionalised sooner. The state would need to put even more resources into their care, and the result would be nowhere near as effective, because family is always family. And that does not serve our community. Caring for the carers. That serves our community.’
Resources and links:
Active Ageing services: https://activeageing.gov.mt/Elderly-and-Community%20Care-Services-Information
European Parkinson’s Disease Association: https://www.epda.eu.com/living-well/caring-and-parkinsons/being-the-carer/
Step up for Parkinsons: https://stepupforparkinsons.com/
Malta Parkinson’s Disease Association – www.maltaparkinsons.com
Paging Dr. AI to Radiology
Artificial Intelligence (AI) is revolutionising the world. We have self-driving cars, algorithms determining future market patterns, and computers diagnosing disease. We believe that AI is supporting huge developments in healthcare.
Continue readingOne size fits… male?
‘Man-flu’ memes and the celebration of women’s endurance hide the reality that the medical world routinely downplays women’s pain and disease. Miriam Calleja takes a closer look.
We often hear that women are more tolerant to pain than men. Many are also proud of it. However, in the famous game-changing paper titled ‘The Girl Who Cried Pain: A Bias Against Women In The Treatment Of Pain’ the authors Diane E. Hoffman and Anita J. Tarzian found that contrary to popular belief, women report more severe levels of pain, more frequent pain, and pain that lasts longer than men’s. Three Maltese women found out the hard way that confiding in medical practitioners does not always lead to help.
Culture and gender frame our behaviour around pain perception. Boys were, and some still are, told not to express pain by crying or showing emotion. Girls were told to calm down and not make a fuss. Pain meant weakness. Our language lacks the vocabulary to adequately describe pain. In ‘On Being Ill’, Virginia Woolf writes: ‘English which can express the thoughts of Hamlet and the tragedy of Lear, has no words for the shiver and the headache… The merest schoolgirl, when she falls in love, has Shakespeare and Keats to speak for her; but let the sufferer try to describe a pain in his head to a doctor and language at once runs dry.’
Gendering pain
By analysing a number of studies, Hoffman and Tarzian found that women are ‘more likely to be treated less aggressively in their initial encounters with the healthcare system until they prove that they are as sick as male patients.’ This is a phenomenon known as the Yentl Syndrome. In other words, doctors may brush female pain off as fabricated or exaggerated. This can impact diagnosis, disease progression, and treatment plans — delaying care and fueling mistrust.
Prescribing uterus removal when a woman was ‘rebellious’ may seem like ancient history, but that bias has not fully retreated. Until the early 1990s, women were mostly excluded from clinical research studies and trials in medicine. What we knew about the body, about disease, and about medicine was based on men. Drugs that didn’t work on men, but might have worked on women, were discarded. With incomplete data, the medical world may have lost opportunities to improve women’s health. Have today’s healthcare professionals been trained to counter this gender bias?
Another doctor later referred Karen for an MRI, and the tumour was detected — a life or death analysis.
Antonia* doubts that. As a teenager she developed digestion problems and nausea every time she ate. When she complained, her family doctor downplayed the problem and suggested that she should just stop eating for a couple weeks. After this shocking response she ignored the issue for a long time, suffering in silence. Another doctor chalked it down to ‘growing pains’ and did not recommend a colonoscopy, even though Antonia asked for it.
Having received no satisfying response from her visits to medical professions, Antonia decided to do her own research, discovering that her symptoms matched the description of a condition called Crohn’s. Because of her constant discomfort and pain Antonia had no choice but to persist until she was granted testing and the correct treatment after years of suffering. This means that two doctors would have left her inflamed digestive system untreated, risking further damage.

‘It is just a phase’
Women are often told that their ailments are due to stress or other emotional factors. A little rest would solve the problem; it is just a ‘phase’. Some doctors would call a woman insisting on referral for further testing a hypochondriac, even in the presence of positive clinical tests (see e.g. Samulowitz et al. 2018 study and numerous articles in the New York Times, The Atlantic and elsewhere). Thankfully, there are enough doctors who look beyond textbook-like symptoms. They make it a point to listen and investigate as much as necessary. Yet the burden of finding a practitioner ready to listen lies with the patient.
Karen visited her gynaecologist complaining of headaches and substantial weight gain. Test results revealed a high prolactin level, which is normally produced during pregnancy or right after giving birth. Yet when Karen asked to be referred for an MRI to investigate for tumours in the pituitary gland, the doctor refused, telling her that she was ‘making a fuss’. Another doctor later referred Karen for an MRI, and the tumour was detected — a life or death analysis.
Some doctors would call a woman insisting on referral for further testing a hypochondriac, even in the presence of positive clinical tests.
Gynaecologists feature often when discussing gender bias. Without systematic training to counter biases, women are left to ‘shop around’ for a gynae that doesn’t shame them or belittle their wishes. This is surprising for a profession specialising in women’s health.
Reproductive issues open another can of worms. Some women who decide not to have children are treated as though they don’t know what they’re doing. Their doctors imply that the patient will inevitably change their mind, or try to guilt the patient into considering the feelings of a hypothetical man they might meet.
You would think that commitment to bear biological children would be respected, but women who undergo IVF are often treated with insensitivity too. Sandra* and her husband had a harrowing story to tell me. Sandra’s gynaecologist decided to immediately hurry her to IVF after the first visit about their concerns at not being able to conceive. The gynaecologist was rarely present for her many appointments at hospital, leaving Sandra to be passed from one doctor to another, internally examined by various doctors without explanation or prior request for consent. With the exception of one doctor, none of them introduced themselves. All along she tried to ask questions, but was kept in the dark about the situation, going along with the doctors’ instructions but losing trust. The outcome of the first procedure was unsuccessful, and because of how traumatising all this felt, the couple decided not to try again.
Unlearning the bias
Pain is subjective and difficult to measure. An individual’s tolerance to pain is affected by various factors, and pain perception may change with time and experience. Pain causes distress, which makes it difficult to measure objectively. So how can overworked doctors make the best possible assessment?
In her thesis titled ‘The Chronic Pain Management Service: Awareness and Perceptions Among Healthcare Professionals’ (University of Malta, 2008), Maria Campbell studied pain perception in other healthcare professions in Malta back in 2008, finding out that outdated attitudes have not been challenged. She writes, ‘Incomplete knowledge, outdated attitudes, myths, and misconceptions about pain and its management contribute to unsafe, inadequate, and inappropriate pain management.’ Medical practitioners wanted to be more up-to-date: ‘The need for information in the form of leaflets, seminars, and continuing education was echoed in the overall answers (90%) of the close-ended question and in the statements declared by participants.’ But before this training becomes systemic, the radical act of listening to women is a good place to start.
* Name has been changed
Further reading:
Fassler, J. ‘How Doctors Take Women’s Pain Less Seriously’. The Atlantic. October 2015.
Hoffman D.E., Tarzian, A.J. ‘The Girl Who Cried Pain: A Bias Against Women In The Treatment Of Pain’. Journal of Law, Medicine & Ethics, Vol. 29, pp. 13-27, 2001.
Campbell, M. ‘The Chronic Pain Management Service: Awareness and Perceptions Among Healthcare Professionals.’ University of Malta. June 2008.
What does health mean to you?
Moving to Malta
Our childhood years are meant to help us develop our sense of identity, belonging, culture, and home. But what happens to those for whom childhood is dominated by moving to a new country with a new language, culture, and social norms? Prof. Carmel Cefai speaks to Becky Catrin Jones.

It’s a small world these days. Developments in technology and transport mean it’s much easier to pack your bags and head off for a fresh start in a foreign land. For many, the destination is Malta. As a beautiful island in the Mediterranean Sea with a booming economy, it is no surprise that it’s drawing the attention of bright sparks and aspiring families from Europe and beyond. In fact, Malta currently boasts the fastest growing EU population.
Of course, it’s not always through choice that you might find yourself leaving your homeland behind. Humanitarian crises and ongoing wars in North and sub-Saharan Africa and the Middle East have seen thousands set sail under the most treacherous conditions in search of safety. For this population, Malta is often the first port of call between the dangers of home and the promise of hope in Europe.
It seems strange to group these populations together, given the stark differences in the journeys that bring them to Malta and the life they seek here. But together, this influx of people has contributed to a sudden rise in interculturalism, where people from different backgrounds interact and influence one another. This is a reality all parties are having to adapt to.
Even in a fairytale scenario, childhood is challenging. Growing up when you’re far from home, look different to everyone around you, and don’t speak their language, makes the challenge reach a whole other level. Children’s wellbeing is an increasingly important and emotive topic to study in Malta, which is a signatory to the United Nations Convention on the Rights of the Child. A team of researchers from the Centre for Resilience and Socio-Emotional Health (University of Malta), set out to explore the situation. They questioned: How do you settle into a new home and identity when you are still trying to figure out who you are and where you are from?
Finding the voices
Children are often a silent group. When analysing the wellbeing or effect of migration on a population, they are usually spoken for by adults. For this study, however, Prof. Carmel Cefai and his team wanted the child’s voice as well. The scope of the study was ambitious; every single contactable, non-Maltese child living in Malta was invited to take part and share their experiences. But this was a challenge.

‘Identifying and obtaining access to foreign children from age zero to 18 was not easy… Some schools suffered from research fatigue and did not wish to participate; whilst translation of instruments and data and use of interpreters drained the limited budget we had for this project.’ Maltese children were contacted and invited to participate too. After all, they are as affected as anyone else when around one in ten of their schoolmates are not Maltese.
The study focused on four main areas; social interaction and inclusion, education, subjective wellbeing and resilience, and physical health and access to services. They covered the experiences of children up to 18 years of age, from various schools, who were either settled into their own family houses or still in open shetlers following a difficult journey to Malta. They also aimed for a balance in migrants’ nationalities; European, North American, African, Middle Eastern, or East Asian; as the experiences of each population are understandably different. Cefai and his team found that the experiences of migrant children in their everyday life are quite positive. In some areas, even more positive than those of Maltese children, with only 8% reporting difficulties in their psychological wellbeing compared to 10% in the native population. Overall, they found that migrant children feel safe, listened to, and cared for by the adults in their communities. Despite the language barriers, most feel like they have a support network, and enough friends though more often than not those friends are other foreign children, not Maltese.They are able to keep up at school, and generally do as well as their Maltese peers, with teachers reporting high levels of engagement.
Adapting to a new world
All is not rosy. Bullying in schools is quite common, though less frequent than that reported by native Maltese children. One in five migrant children also do not feel they have enough friends.
Younger children seem to be more included and engaged than secondary school ones, and in general females fared better in the study than male classmates. That said, age and gender weren’t the main influencers when it came to predicting how well the children engaged at school and in their communities. ‘The study suggests that there are different layers of reality, with the big picture hiding the socio-economic, psychological, and social difficulties encountered by a substantial minority,’ remarks Cefai.
Unsurprisingly, those who speak Maltese feel more engaged than those who don’t, and those who aren’t confident in English are in an even worse position. However, the factor producing the biggest differences between the overall wellbeing, health, and education of the children is their country of origin. ‘The health, wellbeing, and relative comfort enjoyed by many children of European economic migrants contrast sharply with the poverty, poor accommodation, psychological difficulties, learning difficulties, and experiences of discrimination of many children from Africa and the Middle East’, says Cefai. Western Europeans and American children scored highly over all criteria, whereas African and Middle Eastern children are far more likely to be lonely or suffering from social or economic difficulties.
They are more likely to be less proficient in English, which leads to difficulties in making friends with children from other cultures and which also contributes to problems in their education. Although they are generally nourished by their spiritual and religious communities, in all other areas these children report social and emotional difficulties and are also more likely to report facing prejudice and discrimination. Healthcare proved problematic; many parents and children worry that they are subjected to discrimination whilst using services, or do not have enough information to use them in the first place.
A land of opportunity
Despite the additional challenges that these particular migrant children face, the overriding feeling is one of acceptance and hope. Even children in open centres view Malta as a land of opportunity, even when some are in suboptimal housing and lack basic necessities. What children in open centres do not perceive is Malta as their home. Better living conditions in the community, more cultural sensitivity, and openness to interculturalism may help to reduce the feeling of ‘us’ and ‘them’.
So what do Maltese children think? Again, the overall conclusions show that children are open, tolerant, and welcoming of this dramatic and quick rise in multiculturalism that has happened. However, on closer inspection, it seems that there is still a way to go before we can truly call ourselves an open and accepting society.
Relatively few Maltese children have many foreign friends, preferring to spend time with native peers. This hesitation is stronger in children who aren’t from a mixed community, whereas children in independent schools and more exposed to foreign children seem more at ease with the idea that the future might be even more multinational and intercultural. As many as one in three Maltese children also report feeling unsafe in culturally diverse communities, and worry about potential negative consequences of these changes in the future. There also appears to be particular prejudice against children from Africa and the Middle East in contrast to children from Europe, the US, Canada, and Australia.
What has become clear is that both foreign and native children could do with some reassurance. So what do Cefai and his team suggest we can work on to help everyone embrace this new culturally diverse reality?
A united future
‘[We need] to address the needs of marginalised and vulnerable children, particularly those coming from Africa and the Middle East’, says Cefai. There’s also a lot both populations could learn from each other; caring for their environment, sharing cultures, or even adopting healthier lifestyles. By encouraging more open and judgement-free spaces to play, learn, and share, we’ll take away the ‘us’ and ‘them’ ideology from a young age and replace it with one of acceptance, curiosity, and openness to new ideas. This will help prevent the dangerous spiral of segregation and ghettoisation, seen all over Europe.
Cefai suggests a space for more positive role models for those migrant children thrown into a foreign culture that doesn’t seem to have space for them. Having teachers, healthcare workers, or even political representatives who have similar backgrounds will foster this inclusive nature, showing that everyone has a voice when it comes to working together to make this country a home for all.
There’s work to be done with Maltese children. ‘Whilst it is encouraging that the majority hold positive attitudes towards interculturalism, it is worrying that as they grow older children’s attitudes tend to become less positive,’ says Cefai. ‘It’s our responsibility to ensure that educators, community leaders, and parents of Maltese children are part of a national initiative to embrace interculturalism.’
Although overall a positive study, Cefai and team have shown we still have a way to go until every child in Malta feels safe, happy, and at home. And in this ever-changing and diverse environment, Malta has real potential to be an example to its neighbours on how a successful multicultural society can work on every level. These children are our future.
I <3 potato
Plant-based diets are going mainstream all over the world. Cassi Camilleri sheds light on the local vegan movement and how reducing our meat consumption can benefit us all.
Some label the rise of plant-based living as evidence of ‘trend culture’. And they’re not all wrong. Traditional media bombards us with countless headlines on the topic’s pros and cons. Hard-hitting advocacy films like Cowspiracy and Forks over Knives expose the horrors of the meat industry. Social media influencers share their experiences with the diet, turning it into lifestyle content. And now the market is following suit with vegan and veggie lines and options popping up everywhere.
In 2016, an Ipsos MORI survey for the Vegan Society identified that 3.25% of adults in the UK never eat meat in any form as part of their diet, equating to roughly 540,000 people. Vegan January—commonly known as Veganuary—is growing in popularity. This year, a record-breaking 250,310 people from 190 countries registered for the month-long vegan pledge. And Malta is no exception.
While the official number of people following a plant-based or vegan diet are unavailable, interest is clear. Facebook pages Vegan Malta and Vegan Malta Eats have a combined following of over 16,500 people.

The reasons behind people’s decision to take up veganism are various, however three main motivators keep being cited: health benefits, ethics, and environmental concerns. For vegan business woman Rebecca Camilleri the process was natural and gradual. ‘There was no real intention behind it for me. But after a couple of months of following this diet, I noticed that my energy levels were better than before, and this encouraged me to learn more on how I needed to eat in order to nourish my body with the right nutrients to sustain my active lifestyle.’
Researcher and nutritionist Prof. Suzanne Piscopo (Department of Health, Physical Education, and Consumer Studies, University of Malta) confirms that ‘moving towards a primarily plant-based diet is recommended by organisations such as the World Health Organization and the World Cancer Research Fund, for health and climate change reasons.’
Oxford academic Dr Marco Springmann has attempted to model what a vegan planet would look like, and the results are staggering. According to his calculations, should the world’s population switch to a vegan diet by the year 2050, the global economy would save $1.1 trillion in healthcare costs. We would also save $0.5 trillion in environmental costs, all while slashing greenhouse gas emissions by two-thirds.
Despite all this, veganism has earned itself quite a few enemies along the way. The vitriol thrown back and forth across both camps is shocking. Relatively recently, UK supermarket chain Waitrose came under scrutiny after magazine editor William Sitwell responded to plant-based food article ideas from writer Selene Nelson with a dark counter offer—a series on ‘killing vegans’. Sitwell was since forced to resign. Nelson posited that the hostility stems from ‘a refusal to recognise the suffering of animals. Mocking vegans is easier than listening to them.’

Abigail Higgins from American news and opinion website Vox agrees that guilt plays a role in the hatred aimed towards veganism, but also proposes that the whole movement ‘represents a threat to the status quo, and cultural changes make people anxious.’ This notion is based on research on intergroup threats and attitudes by US researchers Walter G. Stephan and Cookie White Stephan.
It however remains a reality that some of the loudest voices in veganism in the past have been militant. Some have invoked hatred and threats towards those that they perceive not to be sufficiently aggressive in promoting the cause. Piscopo calls for a respectful discussion.
‘Food is not only about sustenance and pleasure, but has symbolic, emotional, and identity value. Take meat for example. Some associate it with masculinity and virility. Others link it to food security as meat was a food which was scarce during their childhood. Some others equate it with conviviality as meat dishes are often consumed during happy family occasions. What is important is that we do not try to impose our beliefs, thoughts, and lifestyle on anyone.’
The way forward is a ‘live and let live’ approach, according to Rebecca Galea. When her journey started she had people ‘staring strangely at [her] food’. Even her family didn’t take her seriously. ‘They were very sceptical as their knowledge on veganism was very limited at the time,’ she remembers. Now, seeing the effect the switch has made to Rebecca’s life, her positive choices are naturally impacting theirs. ‘Everyone is free to make their choice,’ she says. Embodying the philosophy of leading by example, Rebecca has even set up her own business making delicious vegan nut butters, spreads, and more, to great success. ‘The more vegan options are available [in Malta], the more people will be attracted to learning and accepting the benefits of veganism. This might also lead to them following a vegan lifestyle!’
With that, and sharing valid, up-to-date research-based information, as Piscopo suggests, it seems there is no stopping this ‘trend’. And who would want to when veganism can lead to a lower carbon footprint and better health for everyone?
Living with a rare disease
Author: Clayton Axiak
Picture yourself waking up one morning with a severe, relentless itch that no clinician or diagnostic tool can understand. Your life would be thrown off kilter. Quality of life would suffer financially, psychologically, and socially as you try to look for a glimmer of light at the end of the tunnel. This is what life is like for most people living with a rare disease.
Often barraged with terms like ‘unknown’ or ‘undiagnosed’, matters can get even more challenging when the condition becomes more elusive or develops life-threatening consequences. And all of this is exacerbated by inequities in treatment and high costs of the few existing drugs that are available.
By EU standards, a rare disease is one that affects fewer than one in 2,000 individuals. And these ‘less common’ ailments are difficult to raise monies for to research, leaving large gaps in scientific and medical literature. One such disease is the poorly understood Idiopathic Hypogonadotropic Hypogonadism (IHH).
Characterised by the absence of puberty and infertility, IHH can be compounded by potentially severe characteristics such as congenital heart disease, osteoporosis at a young age, and early onset of Alzheimer’s disease.
Its cause is usually a genetic anomaly, but a single genetic change can affect two people very differently. This gives rise to an unparalleled complexity that makes the cause harder to decipher. Symptoms are not clear-cut and sometimes mask the actual underlying cause, bringing about misdiagnosis and delayed treatment. Timely diagnosis is crucial for successful treatment that enables the patient to achieve puberty and induce fertility. But this is not always possible.
Under the guidance of Dr Rosienne Farrugia, I am currently analysing and expanding upon a preliminary assessment of IHH in Malta using high-throughput sequencing (HTS) technology (conducted by Adrian Pleven). With HTS, we can read a person’s entire DNA sequence and attempt to identify differences in the DNA code which lead to such diseases.
What the team has found is that some genetic variants typical of IHH are more common in the Maltese population when compared to mainland Europe and African populations. This is likely due to the reduced genetic variation of our population, shaped by successive events of population reduction and expansion throughout our history.
By mapping the genetic cause of diseases prevalent on our islands, we can help medical consultants to employ specific screening tests that are tailored for local patients suffering from IHH. Such advancements in genomic technology and personalised medicine can make a huge impact on people’s lives. And not only to those suffering from IHH; researching one disease, however rare it may be, can shed light on mechanisms that prove useful in treating many others, ensuring that when it comes to health, no one is left behind.
This research project is being carried out as part of a Ph.D. program in Applied Biomedical Sciences at the Faculty of Health Sciences.
To patent or not to patent?
As universities and research institutions look to protect the knowledge they develop, András Havasi questions time frames, limited resources, and associated risks.

The last decade has seen the number of patent applications worldwide grow exponentially. Today’s innovation- and knowledge-driven economy certainly has a role to play in this.
With over 21,000 European and around 8,000 US patent applications in 2018, the fields of medical technologies and pharmaceuticals—healthcare industries—are leading the pack.
Why do we need all these patents?
A patent grants its owner the right to exclude others from making, using, selling, and importing an invention for a limited time period of 20 years. What this means is market exclusivity should the invention be commercialised within this period. If the product sells, the owner will benefit financially. The moral of the story? A patent is but one early piece of the puzzle in a much longer, more arduous journey towards success.
Following a patent application, an invention usually needs years of development for it to reach its final product stage. And there are many ‘ifs’ and ‘buts’ along the way to launching a product in a market; only at this point can a patent finally start delivering the financial benefits of exclusivity.
Product development is a race against time. The longer the development phase, the shorter the effective market exclusivity a product will have, leaving less time to make a return on the development and protection costs. If this remaining time is not long enough, and the overall balance stays in the negative, the invention could turn into a financial failure.
Some industries are more challenging than others. The IT sector is infamous for its blink-and-you-miss-it evolution. The average product life cycle on software has been reduced from three–five years to six–12 months. However, more traditional sectors cannot move that quickly.
The health sector is one example. Research, development, and regulatory approval takes much longer, spanning an average of 12–13 years from a drug’s inception to it being released on the market, leaving only seven to eight years for commercial exploitation.
So the real value of a patent is the effective length of market exclusivity, factored in with the size of the market potential. Can exclusivity in the market give a stronger position and increase profits to make a sufficient return on investment? All this makes patenting risky, irrespective of the technological content—it is a business decision first and foremost.
Companies see the opportunity in this investment and are happy to take the associated risks. But why does a university bother with patents at all and what are its aims in this ‘game’?
Universities are hubs of knowledge creation and today’s economy sees the value in that. As a result, research institutions intend to use and commercialise their know-how. And patenting is an essential part of that journey.
The ultimate goal and value of a patent remains the same, however, it serves a different purpose for universities. Patents enable them to legally protect their rights to inventions they helped nurture and claim financial compensation if the invention is lucrative. At the same time, patent protection allows the researchers to freely publish their results without jeopardising the commercial exploitation of the invention. It’s a win-win situation. Researchers can advance their careers, while the university can do its best to exploit the output of their work, bolster its social impact, and eventually reinvest the benefits into its core activity: research.
At what price?
Patenting may start at a few hundred or thousand euros, but the costs can easily accumulate to tens or even hundreds of thousands over the years. However, this investment carries more risk for universities than for companies.
Risks have two main sources. Firstly, universities’ financial capabilities are usually more limited when compared to those of businesses. Secondly, universities are not the direct sellers of the invention’s eventual final product. For that, they need to find their commercial counterpart, a company that sees the invention’s value and commercial potential.
This partner needs to be someone who is ready to invest in the product’s development. This is the technology transfer process, where the invention leaves the university and enters the industry. This is the greatest challenge for university inventions. Again, here the issue of time raises its head. The process of finding suitable commercial partners further shortens the effective period of market exclusivity.
A unique strategy is clearly needed here. Time and cost are top priorities. All potential inventions deserve a chance, but risks and potential losses need to be minimised. It is the knowledge transfer office’s duty to manage this.
We minimise risks and losses by finding (or trying to find) the sweet spot of time frames with a commercial partner, all while balancing commercial potential and realistic expectations. The answer boils down to: do we have enough time to take this to market and can we justify the cost?
Using cost-optimised patenting strategy, we can postpone the first big jump in the costs to two and a half years. After this point, the costs start increasing significantly. The rule of thumb is that about five years into a patent’s lifetime the likelihood of licensing drops to a minimum. So on a practical level, a university invention needs to be commercialised very quickly.
Maintaining a patent beyond these initial years can become unfeasible, because even the most excellent research doesn’t justify the high patenting costs if the product is not wanted by industry. And the same applies for all inventions. Even in the health sector, despite product development cycles being longer, if a product isn’t picked up patents can be a huge waste of money.
Patenting is a critical tool for research commercialisation. And universities should protect inventions and find the resources to file patent applications. However, the opportunities’ limited lifetime cannot be ignored. A university cannot fall into the trap of turning an interesting opportunity into a black hole of slowly expiring hopes. It must be diligent and level-headed, always keeping an ear on the ground for the golden goose that will make it all worth it.
Science and coffee, anyone?
In an age of misinformation, having a grasp on current affairs and research is essential for us to be active, responsible citizens. Gillianne Saliba writes about the dire need for more dialogue and engagement from citizens and scientists alike.

For many, science is far removed. It’s just a subject they had to take at school. Or the star of crazy stories on newspapers, or videos and memes on social media. Opposing views are a dime a dozen. And sometimes it’s very hard to discern between them; what’s right? what’s wrong? ‘It’s complicated,’ they say, ‘it’s hard’, and so most people move on, letting others do all the talking. As a result, science and citizens have had a rocky relationship. But when the issues being discussed relate to health, technology, and our environment, that is, when they affect us directly, we need to be able to engage.
Science Communication (SciComm for short) can offer a solution to this problem.
SciComm can take many forms. Articles, films, museum exhibitions; you name it. In the wake of a scientific knowledge-gap in the community, SciComm has taken root and has been rapidly growing over the last 40 years. Researchers want to share their ideas and get citizens’ input, gauge interest, and see what others have to say.
Enter Malta Café Scientifique.
To create a safe space where people can chat about science, Malta Café Sci organises monthly science communication events in Valletta where researchers and professionals discuss topics of interest with attendees. Entrance is completely free and open to all, which attracts a diverse audience.

What makes Malta Café Sci special is how it prioritises the public, putting their learning experience first. The events are tailored to them. Speakers keep their talks short and succinct, taking complex scientific concepts and breaking them down, discussing how the research can impact society. The Q&A session that follows is often far longer than the talk itself, opening up a dialogue within the audience. The elitist mantra of ‘it’s complicated’ is so far gone that talks, and the following question and answer portion of the evening, are put to bed with closing drinks where speakers and audience members can have one-on-one time, discussing the topic of the day.
I have been volunteering as an organiser with Malta Café Scientifique for the last nine months. Through the experience, I have gained marketing and public speaking skills.
More importantly, I have had the privilege of a front row seat to pivotal moments in people’s lives—the moment when perception shifts.
I’ve often had audience members come up to me after an event to tell me how the talk changed their ideas. How they are learning to be more receptive but also critical about what they learn and read online. Some point out how they usually steer clear of such events, with many wrongly thinking they aren’t smart enough for them, only to find that they not only understand, but can also participate.
Aside from all this, Malta Café Scientifique is also conducting its own research. Led by Café Sci’s project manager Danielle Martine Farrugia, we are evaluating and interviewing different science communicators about their practices. We’re also evaluating the initiative to understand its contribution to science communication in Malta.
What we can already see is that Malta Café Sci is living, breathing proof of how people can come together when dialogue is open and welcoming. It is empowering local researchers to share their findings with citizens while giving community members the chance to learn and weigh in on work that may have ramifications for them. Where a learning process is no longer from expert to layman, but a continuous sharing of information in both directions.
Note: For more about Malta Café Scientifique’s next events, or if you want to get involved, see its Facebook page or Instagram @maltacafesci. Or email us on cafesci@mcs.org.mt.