Local researchers from the DRIFT (Dense Recording of In-Shoe Foot Temperatures) project team are investigating foot health in patients with diabetes. In collaboration with Mater Dei Hospital, researchers are developing smart insoles, a system with embedded thermal sensors that measure foot temperatures. THINK got in touch with Chiara Modestini, podiatrist and researcher with DRIFT, to find out more.
The Covid-19 pandemic disrupted various outpatient and primary health care services locally. Health professionals were only able to attend to urgent cases, and only after a risk assessment was determined over the phone. Restrictive measures were implemented to curb the spread of the virus, and people were advised to remain indoors unless absolutely necessary. Fear and anxiety has kept many from setting foot in a hospital or clinic, even in an emergency situation. Combining this with back-logged appointments and health care professionals falling ill, the result is a strained healthcare system.
A New Type of Healthcare
Since the Covid-19 outbreak, novel approaches such as telemedicine and virtual consultations have been implemented locally. Telemedicine refers to the practice of caring for patients remotely through telephone or video chat. However, when virtual consultations are not sufficient, other approaches are needed.
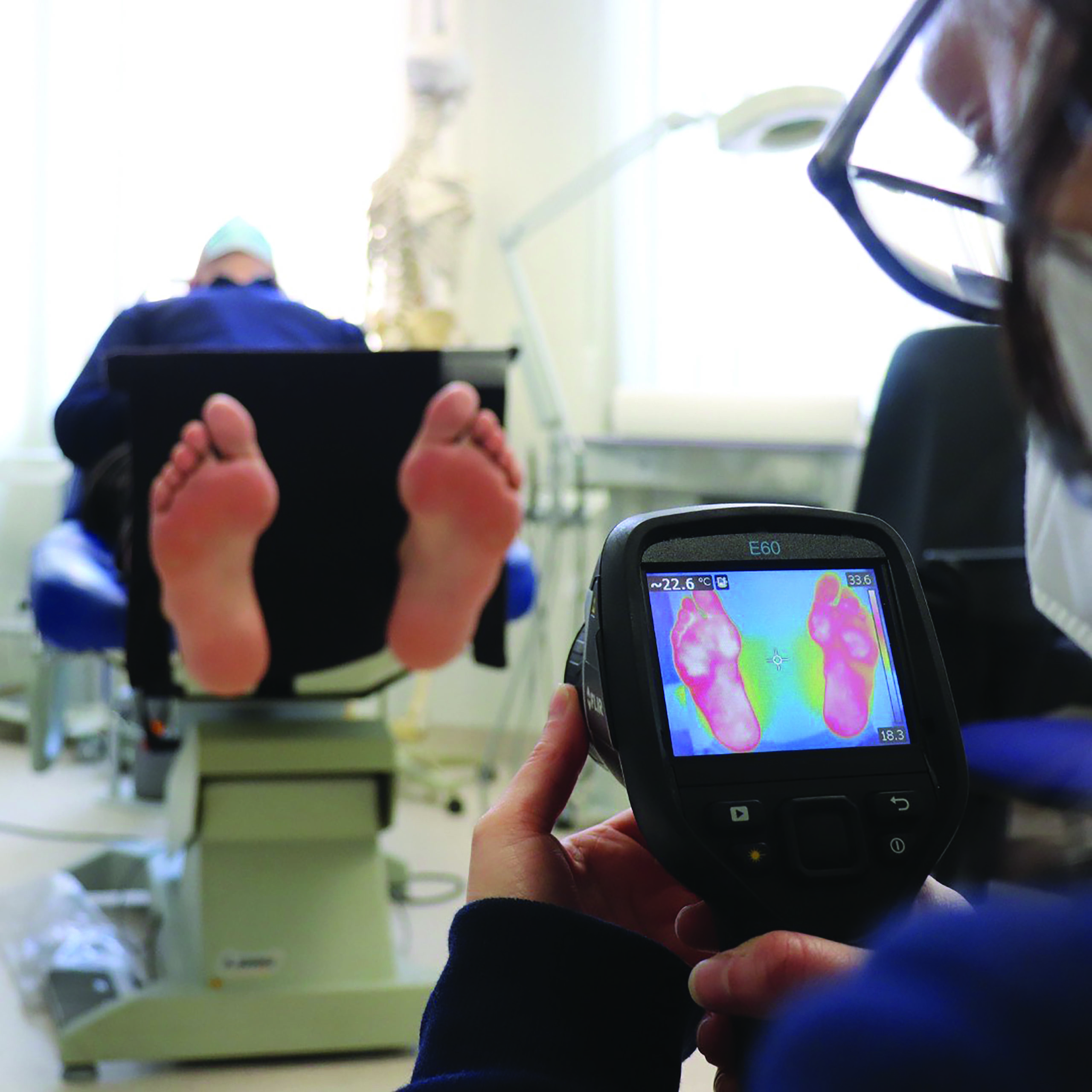
Researchers at the University of Malta (UM) in collaboration with Mater Dei Hospital are currently developing smart insoles with embedded thermal sensors that interact with the sole of the foot. The Dense Recording of In-Shoe Foot Temperatures (DRIFT) Project is led by Dr Stephen Mizzi (Department of Podiatry, UM), Dr Owen Falzon (Centre for Biomedical Cybernetics, UM), and Prof. Kevin Cassar (Department of Surgery, Mater Dei). Together with the rest of the team, they have developed insoles that are able to detect temperature changes in a patient’s feet.
This information is provided in real time to both the user and clinician, allowing the clinician to monitor the patient’s progress. The technology could overcome the challenging self-care practices diabetics need in their daily routine.
DRIFT and Diabetes
Providing care for people living with diabetes is extremely crucial in these challenging times, especially when having foot-related complications places them in a high-risk category. When glucose levels are not controlled, complications may arise. For instance, damage to the foot’s nerves and blood vessels would cause sensory loss and poor circulation. Of all the complications of diabetes, those involving the feet have normally required substantial face-to-face patient visits to healthcare clinics for screenings and treatments, such as checking circulation and nerve status and treating ulcers. If the patient is not checked by a medical professional or themselves, then major foot complications such as ulcers and limb loss can occur.
These smart insoles are able to provide wearers with peace of mind, knowing that even though they may not be able to access frequent physical podiatric healthcare, their podiatrist will still be able to monitor and intervene.

In September 2019 the DRIFT project team ran a survey on 300 diabetic patients. The study found that 37% of diabetic patients visit a podiatrist approximately six times a year or more. These numbers have dropped significantly over the last few months due to the global pandemic. Low visitation numbers are problematic since only 48% of patients living with diabetes check their feet every day, 55% do not check their feet after performing physical exercise, and 52% are not aware of skin injuries during exercise. Patients need a way to check their feet.
Non-ulcer diabetics (diabetics that do not have ulcerations in their feet) benefit from walking. It helps to better control glucose levels and improves blood flow to the feet. However, exercise can also harm diabetic patients. During walking, friction between the sole of the foot and the inside of the shoe may pose a major threat on the lower limbs, especially in diabetics with poor circulation or loss of sensation, as they are more susceptible to skin breakdown and ulceration. This is where the smart insoles truly shine.
Bridging the gap between self-care and health care
The smart insoles being developed can be used at all times during daily activities. These smart insoles are able to provide wearers with peace of mind, knowing that even though they may not be able to access frequent physical podiatric healthcare, their podiatrist will still be able to monitor and intervene. Patients will be able to exercise safely as advised by their health care professionals, knowing that if at any point they are in danger, they will be alerted through an app on their phone, helping them to immediately stop their ongoing activity.
The smart insoles should transform diabetes patients’ lives. It helps clinics devise better care to prevent injury and reduce the number of ulcerations and amputations. Most importantly, it will eliminate fear from the equation and allow patients to feel safe — so important in these times. This novel approach will bring a paradigm shift in diabetic foot care, bridging self-care and health care.
Chiara Modestini is a podiatrist and researcher forming part of the DRIFT project, together with Tiziana Mifsud. The project is funded by the Malta Council for Science &Technology (MCST), for and on behalf of the Foundation for Science and Technology, through the Fusion: R&I Technology Development Programme.
Further Reading
Shin L, Bowling FL, Armstrong DG, Boulton AJM. (2020). Saving the diabetic foot during the COVID-19 pandemic: a tale of two cities. Diabetes Care.,43:1704–1709
Centre for Biomedical Cybernetics. (2021). Dense Recording of In-Shoe Foot Temperatures (DRIFT). University of Malta. retrieved from:https://www.um.edu.mt/cbc/ourprojects/drift




Comments are closed for this article!