Contraception, and especially the contraceptive pill, have revolutionised society in the past 60 years. Yet one of the most utilised methods has side effects that are still not addressed by science worldwide, and shining a light over Malta shows a lack of data on the population’s reproductive health. THINK investigates.
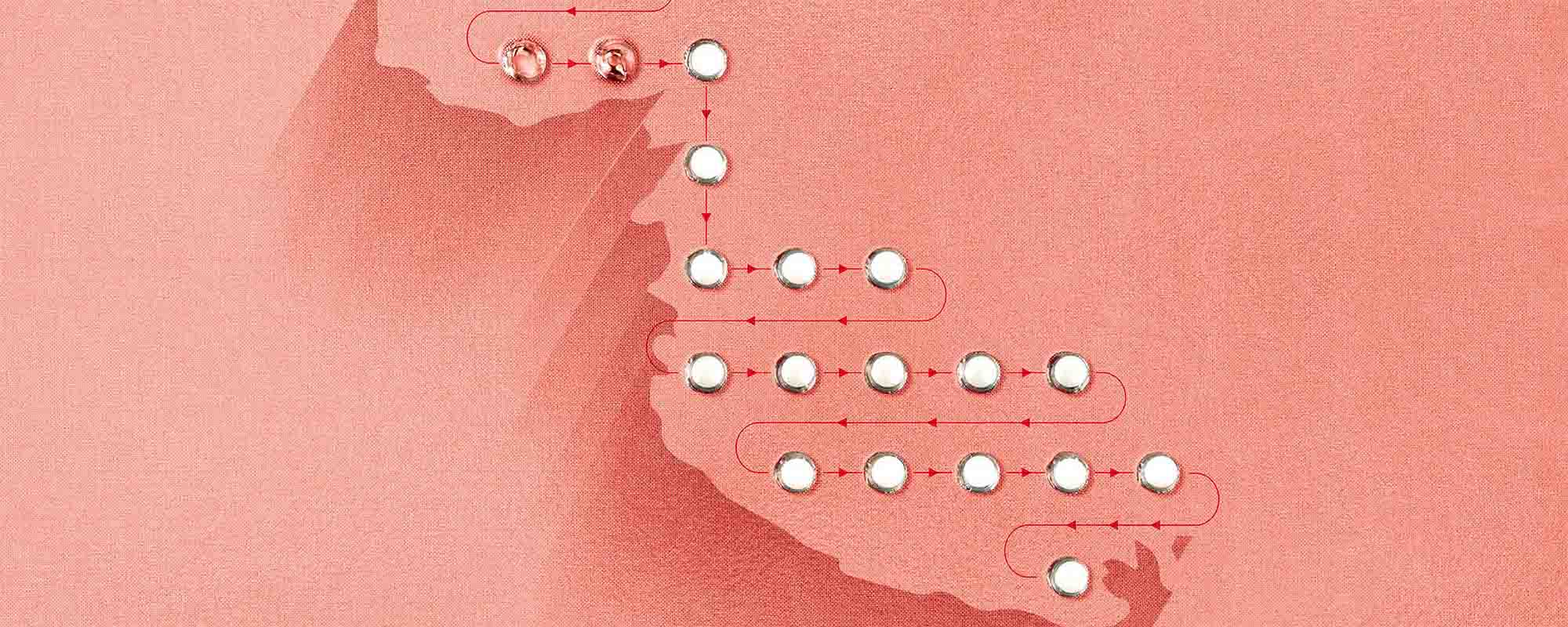
Condoms, hormones, coitus interruptus; there are many contraceptive methods available to prevent pregnancy, with variable rates of efficacy. According to the United Nations (UN) 2019 report, in Europe, the main forms of contraception used are the male condom (17.8%) and the pill (14.6% of women). With over 100 million users, the contraceptive pill is the most used hormonal method worldwide.
The Good
‘The pill wasn’t just socially revolutionary. It also sparked an economic revolution – perhaps the most significant economic change of the late 20th Century,’ explains Tim Harford on the BBC column 50 Things That Made the Modern Economy. More than preventing unwanted pregnancies, the introduction of the contraceptive pill in the 1960s also contributed to women’s sexual and social emancipation.
For the first time, women had the power to control their reproductive health independent of their partner, giving them the ability to choose when to have children. As Harford put it, ‘using a condom meant negotiating with a partner. […] But the decision to use the pill was a woman’s, and it was private and discreet.’ The ability to control their sexual health opened space for women to pursue educational opportunities, build careers, and achieve economic independence.

Although the action mechanisms of the contraceptive pill are well understood, there is still a tremendous gap in knowledge about its side effects. There isn’t much research exploring the impact of the contraceptive pill on the behaviour and psychological well-being of women.
The pill is an oral hormonal method that prevents pregnancy, but not sexually transmitted diseases – only male and female condoms prevent these infections.
Prof. Isabel Stabile, an academic at the University of Malta and a general gynaecologist for the last 40 years, explained to THINK the differences between the two main types of contraceptive pill in the market: the combined pill and the minipill.
The combined pill has a mix of the hormones oestrogen and progesterone, preventing ovulation. Brands have combination pills with either different types of progesterone or different doses of oestrogen.
Some pills, called minipills, only contain progesterone and prevent pregnancy by making the cervical mucus thicker and the lining of the uterus thinner. Minipills with higher concentrations of progesterone can also stop ovulation, but unlike the combination pill, the minipill is not usually used for hormonal regulation.
Apart from birth control, the contraceptive pill can also help with many health conditions, such as migraines (although it can also cause migraines in some cases), menstrual pain, endometriosis, heavy menstrual flow, or acne. The pill is also linked to a lower risk of ovarian, endometrial, and colon cancer, and is an essential mechanism to treat polycystic ovarian syndrome.
The Bad
However, no medication comes without its risks. The main side effects of the pill include weight gain, loss of sexual libido, and mood swings. Rare side effects include a higher risk of thrombosis and pulmonary embolism.
Stabile reveals that most of her patients in Malta worry about weight gain, irregular bleeding, changes in body hair, and the contraceptive not working. She also confirms that some types of contraceptive pill can cause mood changes, vaginal dryness, and loss of libido.
In her practice, Stabile tries to regulate the side effects by changing the doses of hormones. Because there are several different types of combination pill on the market, physicians can tweak the dosages to control patients’ side effects. Other consequences can be tackled with different mechanisms. For example, vaginal dryness can be addressed by using lubricants.
The Ugly
Changes in cognition and decision making, as well as deterioration of emotional well-being, have been reported as possible side effects of the pill.
Regardless of the side effects encountered, Stabile believes that information and awareness is the most important element. ‘In Malta, more people need to know about the side effects of the pill. There is a lack of information,’ she explains.
The UN have recently given similar advice to Malta. After the visit of a working group on discrimination against women and girls in July of 2023, a report stated: ‘comprehensive sexuality education is central to preventing teenage and unwanted pregnancies but also in the prevention of sexually transmitted diseases and gender-based violence.’ The UN recommended that Malta review its awareness strategies, especially sexuality education in schools.
The side effects addressed so far reduce the quality of life of those who get them and are the reason why one third of women stop taking the pill in the first year. Yet there are other side effects that are understudied.
Changes in cognition and decision making, as well as deterioration of emotional well-being, have been reported as possible side effects of the pill. Users of the contraceptive pill also seem more likely to have depression and anxiety. Women have reported debilitating migraines that lead to seizures, and besides changes in libido, some research (not all) shows alterations in sexual attraction.
It is worth mentioning that all these side effects have previously stopped the developement of a male contraceptive pill. These small-to-hefty side effects can also be found in other hormonal contraception methods, such as the patch, hormonal intrauterine devices (IUD), or the vaginal ring.
The Case of Malta
From the 1980s until 1992, Malta had free, state-run family planning clinics where women could go to get advice on their reproductive health. In 1993, the clinics closed, and nowadays, women can either pay to go to their family doctor or gynaecologist, go to a Public Health Centre and talk with a general practitioner (who, according to Stabile’s experience, may not always be comfortable with giving contraceptive advice), visit the weekly Well Woman clinics at the Public Health Centres, or get directed to the gynaecology speciality at Mater Dei Hospital. Getting access to the services at Mater Dei, however, takes a long time, and it’s designed for complications, not for prevention measures such as the pill. Most of the state services have a long waiting list, so most women prefer to go to the private sector.
There is no freely available contraception in the public health system, and only emergency contraception and condoms are available at pharmacies without a doctor’s prescription. Contraceptives are also not covered by the state’s health insurance, and free condoms are only handed out by non-profit organisations like Doctors for Choice. According to the UN working group’s report, the lack of access to free contraception pushes women to forgo protection and rely on coitus interruptus (which they do not consider a contraceptive method). They advised the state to provide free contraceptives to certain groups.
Malta also has a lack of official data on the population’s contraception usage, unplanned pregnancies, miscarriages, or abortions. Most of the information available online comes from reports from international organisations or small academic studies, and the information we do have is not optimistic.
Malta’s relationship with contraceptives seems dire, which considering the need to upgrade sexual education at schools, the lack of public awareness towards safe sexual practices, and the existence of methods with so many misunderstood side effects, comes as no surprise. The upside is that, by empowering the population with correct information, good practices can become the norm.
When it comes to the contraceptive pill, researchers and pharmaceutical companies need to continue the work to understand its impact on women’s health, so we can empower women to reap the benefits of their reproductive rights.
Editor’s Note: While preparing this article, we realised that there is a lot that needs to be said. We prepared a separate article which looks at the pill beyond Malta. Specifically, we examine why there is such limited research funding when it comes to contraception. Check it out here.
Further Reading
BBC. (2022, February 24). “it sucked”: Eight women open up about being on the pill. BBC Future. https://www.bbc.com/future/article/20180823-women-speak-about-side-effects-of-the-birth-control-pill
Blake, K., Arthur, L., & Casto, K. (2020, October 2). How is the contraceptive pill affecting your mood?. Pursuit. https://pursuit.unimelb.edu.au/articles/how-is-the-contraceptive-pill-affecting-your-mood?fbclid=IwAR0zAEsP5no-mQxODEujQC6d7fBGplnHRCp99Z–QJ6jxW47sIt3HmidTTw
Britton, L. E., Alspaugh, A., Greene, M. Z., & McLemore, M. R. (2020, February). CE: An evidence-based update on contraception. The American journal of nursing. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7533104/
Browne, G. (2022, June 22). Do birth control pills affect your mood? scientists can’t agree. Wired. https://www.wired.com/story/do-birth-control-pills-affect-your-mood-scientists-cant-agree/
Contraceptive use by method 2019: Data Booklet. (2019). United Nations.
Crockford, K. (1992). Family Planning in Malta. um.edu.mt. https://www.um.edu.mt/library/oar/bitstream/123456789/47794/1/Family_planning_in_Malta_1992.pdf
Fenech Conti, F. (2022, August 1). Family Planning and contraception practices of Maltese women. L-Università ta’ Malta. https://www.um.edu.mt/library/oar/handle/123456789/111389
Harford, T. (2017, May 21). The tiny pill which gave birth to an economic revolution. BBC News. https://www.bbc.com/news/business-39641856
Hill, S. E. (2020, March 26). Feel like a different person on the pill? here’s how it affects your mood. ideas.ted.com. https://ideas.ted.com/how-the-birth-control-pill-affects-your-mood/
Jones, B., Hahn, A., Fisher, C., Wang, H., Kandrik, M., Han, C., Fasolt, V., Morrison, D., Lee, A., Holzleitner, I., O’Shea, K., Roberts, C., Little, A., & DeBruine, L. (2018, April 30). No compelling evidence that preferences for facial … – sage journals. https://journals.sagepub.com/. https://journals.sagepub.com/doi/10.1177/0956797618760197
Swift, B., & Becker, C. (2023, June 8). Birth control continues to fail women – so why has nothing changed?. The Conversation. https://theconversation.com/birth-control-continues-to-fail-women-so-why-has-nothing-changed-164195
Wenner, M. (2008, December 1). Birth control pills affect women’s taste in men. Scientific American. https://www.scientificamerican.com/article/birth-control-pills-affect-womens-taste/Zethraeus, N., Dreber, A., Ranehill, E., Blomberg, L., Labrie, F., Schoultz, B. von, Johannesson, M., & Hirschberg, A. L. (2017, April 19). A first-choice combined oral contraceptive influences general well … https://www.fertstert.org/. https://www.fertstert.org/article/S0015-0282(17)30247-9/fulltext
Author
-

Antónia was a Biologist, once upon a time. She transitioned from the glamorous world of lab benches and international conferences to her one true love - Science Communication. Antónia works as a freelance science writer and also manages social media for THINK. In her free time, she pets street cats and educates people on Portuguese gastronomy - often against their will.
View all posts





Comments are closed for this article!