Cancer behaviour is highly complex. Tumour cells are adept at evading the body’s defence mechanisms and therapeutic drugs over time. At Mater Dei Hospital, a multidisciplinary team of health professionals is analysing a rare case of cancer cell transformation that may uncover new therapeutic approaches for patients with this cancer type.
For anyone in the biomedical field, cancer is scary and fascinating in equal measure. It shows the wonders of life and how a cell can modify itself to survive the most inauspicious conditions. A cancerous cell is, in its most basic form, an unparalleled survivor – destroying the very ecosystem that enables its existence.
A big part of cancer research tries to understand how cancer cells mutate and adapt to continue to proliferate: how a tumour evolves to keep growing, camouflages itself from the immune system, and at times persists after therapy. In some cases, one cancer type even transforms into another. In fact, researchers at Mater Dei Hospital are studying how a particular cancer has metamorphosed.
A Metamorphosis
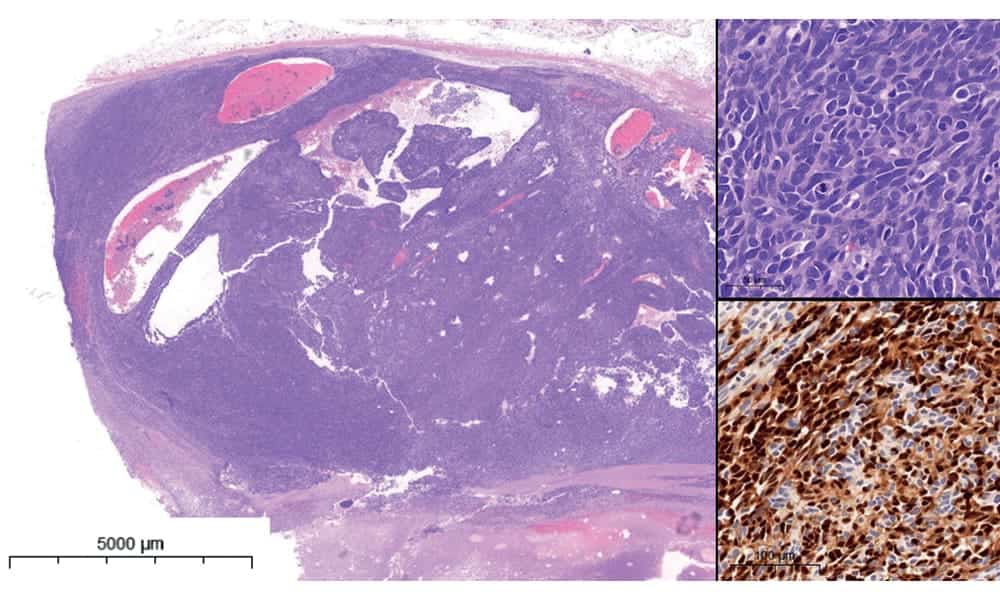
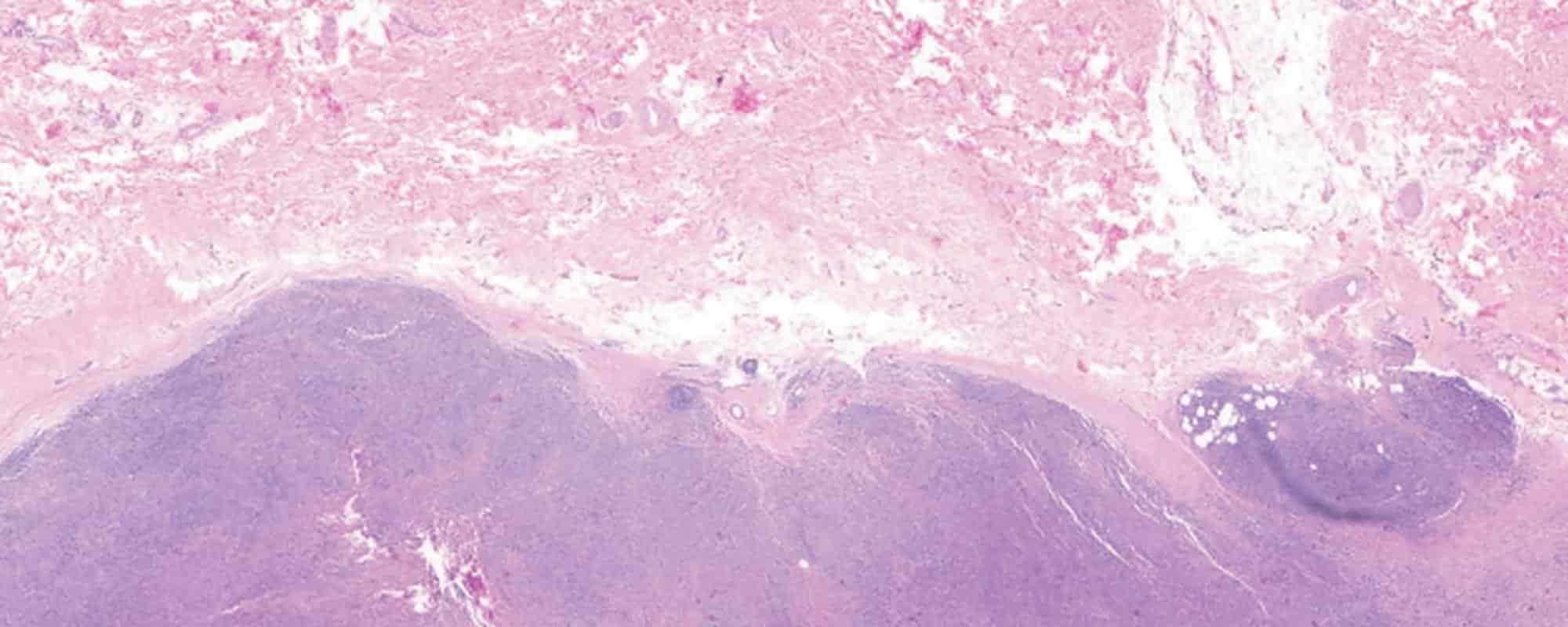
Melanoma (skin cancer) is an aggressive cancer that can form metastases (cancer cells migrating from the initial tissue to a new location) in nearby skin or even distant organs. A team of pathologists and biomedical scientists from the Cellular Pathology and Molecular Pathology & Genetics Laboratories within the Department of Pathology at Mater Dei Hospital (MDH), are studying a particular case of melanoma. A few years after presentation and treatment, the melanoma migrated to a lymph node and transformed into a neuroendocrine tumour. This type of cancer, unlike melanoma, is more like the cells that are found in glands, rather than in skin.
This process, in which one cell type becomes another, is called transdifferentiation. Although neuroendocrine transdifferentiation is known to occur in certain types of cancers, it very rarely occurs in cases of skin cancer. Transdifferentiated neuroendocrine tumours are usually highly aggressive and easily evade current therapies.
As such, this research team is committed to understanding the molecular process that led to the transformation of a melanoma into a neuroendocrine cell. By doing so, they want to know how melanoma turns into a neuroendocrine tumour and use this information to develop new targeted therapies.
The Genetics of Cancer
Cancer cells multiply uncontrollably, as their growth signals are forced to remain ‘ON’ through mutations in what we refer to as driver genes. Genes form the code for proteins that a cell produces to be able to survive and perform its functions. In the case of cancer cells, researchers refer to gene defects that cause the cell to become cancerous as driver genes. By identifying the possible driver genes of the neuroendocrine tumours, the researchers may understand which proteins to target in order to kill the cancerous cells. This can then be tested in cell experiments where cancer cells can be treated with candidate drugs to observe the effects.
Using cancer tissue biopsies along the progression of the cancer, the group is looking for driver gene mutations that may cause gene upregulation, downregulation, or inactivation. An upregulated gene is used more times, so the cell will have a higher concentration of the protein it encodes, while downregulation is the opposite, and inactivation switches the gene off entirely. These changes alter the cell’s activities, which led to the transformation into neuroendocrine tumour cells.
This targeted approach may decrease secondary effects as opposed to general treatments such as chemotherapy, which disrupts both healthy and malignant cells. If a drug targets proteins that are primarily expressed in the cancerous cells, the drug won’t cause such strong systemic effects typically encountered in traditional chemotherapy, but cancer cells will be more adversely affected.
To find the driver genes, the researchers used whole-genome sequencing of the tissues from the original melanoma, the metastases, and the neuroendocrine tumour to find mutations exclusive to the neuroendocrine cells. The exclusively mutated genes will then be compared to data for other neuroendocrine tumours available through online databases to help identify potential drivers of this cancer type.
Research for Better Healthcare
Securing funding was essential to carry out this analysis, and the project has been funded through a research excellence grant by MCST. With the funding, the Cellular Pathology Laboratory at MDH recruited laboratory scientists from the hospital to perform research work and gain valuable experience in research methods and also bioinformatic analysis of genomes.
The research group outsourced the bioinformaticians to process and analyse the data obtained from whole-genome sequencing and the comparisons with the online databases. This research project required a multidisciplinary team of healthcare professionals, including dermatologists, biomedical scientists in the fields of molecular pathology (those who analyse genetic changes during life that led to cancer) and cellular pathology (those who analyse the tissues and morphological alterations to the cells), as well as bioinformaticians.
The collaboration between healthcare fields is enabling a better understanding of cancer behaviour for the development of personalised therapies for an aggressive cancer type and allowing a better understanding of cancer, highlighting the importance of investing in healthcare-driven research.
Glossary
Metastasis: when cancer cells migrate from the initial tissue to a new location
Neuroendocrine tumour: a rare type of tumour that affects cells that release hormones into the bloodstream
Transdifferentiation: A process in which one cell type transforms into another
Upregulated: the process by which a cell increases its response to a substance or signal from outside the cell to carry out a specific function
Beyond Academia is our newest addition to the magazine. In this section, we feature research connected to Malta conducted by institutions or individuals not linked with UM or other academic organisations.
The Project: “Molecular switch underpinning Neuroendocrine Transdifferentiation in malignant neoplasms – MOLNET” (REP-2021-021) is supported by the Research Excellence Programme (REP) funded by the Malta Council for Science &Technology (MCST).





Comments are closed for this article!